The Touch Issue


Physical Touch
It’s the first sense we develop — our most direct contact with the world around us. And we lost so much of its benefits during the pandemic.
Physicians and therapists, scientists and scholars are diving deep to better understand the role that touch plays in our mental and physical health.
What can we learn from the art and science of touch?
By Erin Howe
Jennifer Schultz was about to receive life-altering news. Then 43 years old, Schultz was sitting in her doctor’s office in a downtown Toronto hospital. She was about to find out she had Stage 3 lobular breast cancer, an invasive disease that can be difficult to diagnose.
The diagnosis would turn the world as she knew it upside down. It would lead to radiation, two surgeries and eight rounds of chemotherapy.
“When you give someone a serious diagnosis or let them know they have a chronic condition, their lives could be upended, even if it’s not life-threatening,” says Schultz, now 51 and in remission for six years.
Schultz decided to use her experiences as a cancer patient for good. She speaks regularly about patient-centred care in the Patient as Teacher program for the Temerty Faculty of Medicine’s surgical clerks. The program — set up in 2016 — provides third-year MD students in their surgery rotation with an opportunity to learn directly from patients.
“In moments like these, don’t underestimate the power of a gentle touch and asking, ‘Are you OK?’” she says.
For Schultz, it’s a chance to remind learners of the power of physicians to impact a patient in their most difficult moments.
Jennifer Schultz says in-person conversation can be a comfort to people receiving a difficult diagnosis. (23 sec)
The work Schultz does has become even more urgent to her as phone and virtual appointments become more ingrained in the health care system. Her experiences have made it clear to her that some discussions with health care providers should only happen in-person, and that the role of touch is crucial.
What Schultz is expressing is something that some health care practitioners are hearing more broadly across the board. The question of what is gained — and what is lost — in the advent of virtual care is of central importance to Canadian patients and the health care community.
By all accounts, the COVID-19 pandemic led to an unprecedented surge in virtual medical care. A 2022 report by the Canadian Medical Association, the College of Family Physicians of Canada and the Royal College of Physicians and Surgeons of Canada shows that rates of virtual care skyrocketed from 10 to 20 per cent of all health care visits in 2019 to 60 per cent in April 2020. By 2021, that percentage had fallen to 40 per cent of all visits, which is still significant.
“The [costs of physical contact] have been made manifest by the COVID-19 pandemic and have forced mass adoption of virtual care across Canada years ahead of schedule,” according to a 2020 C.D. Howe Institute report. “Virtual care will be a mainstay of clinical care in the future. There is the potential to transform the patient and provider experience, lower costs and improve care, particularly for those with chronic diseases.”
For a health care system with overwhelmed emergency rooms and rising wait times to see specialists —as well as a shortage of primary care doctors — virtual care could be seen as a way of leveraging resources.
But the rise of virtual care could also leave some people behind, says Tara Kiran (MD ’02), an associate professor in Temerty Medicine’s Department of Family and Community Medicine and the Fidani Chair in Improvement and Innovation.
In a study early in the pandemic, Kiran and colleagues found that people with a low income or poor health, or who had immigrated to Canada within the last 10 years had a stronger preference for in-person care. Issues such as language barriers and privacy concerns may have contributed to these feelings.
“If done right, virtual models can enhance equity and access care. But if not, we might inadvertently create additional barriers for some patients,” says Kiran, who practises family medicine at Unity Health’s St. Michael’s Hospital.
Further research by Kiran and others compared outcomes for patients who sought virtual care from their own physician with those who received care from a physician as part of a virtual-only care service, akin to a virtual walk-in clinic. People who saw their own doctor were less likely to visit the emergency room afterward than if they’d seen a doctor online who they had no prior relationship with and wouldn’t see again. While Kiran acknowledges that virtual care can have its advantages, she’s heard from many patients who want to see their doctor in-person.
Kiran was the principal investigator of the 2024 OurCare final report, the largest initiative to engage Canadians on the future of primary care. Over 16 months, Kiran and colleagues gathered more than 9,000 survey responses, and convened five provincial priorities panels and 10 community roundtables.
Kiran says that the findings show that most people still want to see their primary care clinician in-person. The majority of respondents also said they want virtual care in addition to office visits and the ability to make that choice themselves.
The finding doesn’t surprise Nazik Hammad (MSc ’95), a Temerty Medicine oncology professor. During treatment, there can be an information asymmetry between patients and physicians, she says, and being in the same room can help communication. Physicians understand the care plans for their patients, but the information can be a lot for people to take in, adds Hammad, a Unity Health oncologist.

“In person, I have extra opportunities to ensure my patients understand what I tell them,” Hammad says. “If I notice someone doesn’t take notes or ask questions, I might say something like, ‘I told you about this medication’s side effects. Would you be able to tell me what you remember from what we discussed?’”
Though patients may bring a family member or friend to their in-person appointments, Hammad points out that’s less likely to happen with phone appointments.
“Patients can benefit from having a support person who can help digest and remember information, advocate for them, and provide reminders to help ensure adherence to medication or other treatment plans,” says Hammad.
Virtual care can also help people before and after complex procedures, says Lisa Wickerson (BScPT ’93, MSc ’12, PhD ’19), an assistant professor in Temerty Medicine’s Department of Physical Therapy.
In 2019, Wickerson began researching hybrid rehabilitation programs to support people waiting for or recovering from a lung transplant. Before 2020, transplant patients attended hospital sessions three times a week pre- and post-procedure for supervised assessment and exercise training.
“When care is so specialized, in a way, that can be a rationale to keep it on site,” says Wickerson, who is also an affiliate scientist at University Health Network’s Ajmera Transplant Centre.
She now studies hybrid rehabilitation, in which patients receive both in-person and virtual care before and after a lung transplant, exploring how to assess and monitor a patient’s condition as they prepare for or recuperate from the surgery. Though a growing number of people already use wearable technology, such as a smartwatch, Wickerson says there is a need for accurate tools validated for at-home medical use.
Currently, Wickerson is finding ways to create program delivery models that can be personalized for individual needs and risk factors, which combine in-person and virtual care. She sees the promise in both approaches to help patients meet their needs.
“There’s no one-size-fits-all approach. We need different pathways for people based on their functional capabilities and medical status, in terms of what kinds of alerts, reminders and supervision they may need during preparation or recovery,” Wickerson says. The advantages of time management offered by virtual connection can extend to education as well.
In 2021, the Patient as Teacher program switched from an in-person model to online during the pandemic. Four years prior, the program had begun as a way of giving students an unvarnished view of the full experience of people with breast cancer. Over two sessions, cancer survivors came in-person to share their personal stories and perspectives with medical students.
The pandemic meant online sessions became necessary. At first, program founder and surgeon Jory Simpson (PGME ’12) says he was skeptical about how well online delivery of the program would work. But his skepticism lifted as he saw the program’s continued success with learners.

“It almost felt disrespectful because I believed so much in the in-person connection between patients and the learners. I worried it would be a negative experience for the patient-teachers,” says Simpson, an assistant professor in Temerty Medicine’s Department of Surgery, who launched the program.
Simpson says it didn’t take long to see the merits of moving things online.
“Students can engage with the patient-teachers in a professional and meaningful way. They can still gather in small breakout rooms for more intimate conversations,” says Simpson, who practises at Unity Health. “The students learn how to create online connections and get that practice with a patient population.”
Enabling volunteers to log in to their teaching sessions has also allowed a more diverse pool of cancer survivors to participate — including people who live outside of Toronto and people who have less financial privilege.
“We can recruit people from a wider range of geographic and socio-economic communities,” notes Simpson. “They don’t need extra time off work to travel, or worry about taking transit, or driving and finding parking in downtown Toronto.” Other Canadian medical schools have replicated the Patient as Teacher program, and online sessions are now available to postgraduate medical learners.
“We’ve seen learner perspectives of a surgeon’s most-important attributes shift dramatically,” says Simpson. “Before these sessions, all of the students ranked technical skills first. When asked again after the Patient as Teacher program, humanistic traits like compassion and the ability to provide comfort were given much more weight.”
Professor Danielle Martin says in-person and virtual interactions are both important in the relationship between family doctors and their patients. (44 sec)
And what if, as Danielle Martin (PGME ’05) puts it, it’s “not an ‘either/or situation, but a both/and’ approach?”
Relationships are the most valuable tool that family physicians have, says Martin, chair of the Temerty Medicine’s Department of Family and Community Medicine. She says that over time, primary care providers build trust, and learn to pick up on verbal and non-verbal cues to better gather information and sense when more is going on than a patient communicates or even realizes.
Martin, who is also a family physician at Women’s College Hospital, says the physical examination itself can help put patients at ease.
“When done well, it can be reassuring,” says Martin. “The respectful laying on of hands can help patients feel cared for, seen, and that their doctor is fully focused on them. The consent someone gives for physical touch in a joint pursuit of health is sacred.”
Despite this, Martin says virtual care has become a key part of the integrated relationship between doctors and patients. Connecting by phone to check in on how a treatment plan works for a patient, review test results or provide a requisition for a regular procedure such as a mammogram or blood work are all instances in which virtual care can be appropriate.
People who live in rural and remote areas or who belong to marginalized groups may also benefit.
Some people avoid the health care system because of negative past experiences or valid fears of racism, Martin says. Facilitating remote access, particularly if it enables access to a clinician from someone who belongs to the same community, for example, can help.
“There’s room for all the tools,” she continues. “They’re all manifestations of an ongoing commitment to the relationship between a health care team and the person in pursuit of good health.”
Schultz agrees. Though caring touch has its places, in real life so does the virtual empowerment of patients, she says. “Virtual care is just another way medicine is advancing. And it can help put patients in the forefront of their own care.” •
The OurCare Report and its findings
A recently released report examining the state of primary care in Canada has findings that directly address the future of virtual care.
Tara Kiran, the study’s principal investigator, led the research, which is the largest-ever engagement of the public about primary care in Canada.
The OurCare final report contains insights from a survey of more than 9,000 people in Canada, and those gleaned from conversations with more than 350 members of the public during five provincial panels and 10 community roundtables.
The report, published in February 2024, reveals that Canadians would like:
Source: OurCare final report

By John Lorinc
When Alainna Jamal (PhD ’20, MD ’22) ponders the threats that truly worry her, she focuses on one particular statistic in the unfurling story of the spread of CPE (known more formally as carbapenemase-producing Enterobacterales), an antibiotic-resistant pathogen that attacks almost any system in the body and is rapidly gaining a foothold in Canadian health care settings.
Interestingly, the detail she mentions isn’t a fatality rate that can run up to 50 per cent.
Rather, Jamal, a second-year internal medicine resident at the Temerty Faculty of Medicine, is preoccupied with the way the pathogen is proliferating.
The germs are transmitted through touch via the unwashed hands of health care personnel, contaminated medical equipment and splash from hospital sink drains.
Though commonly associated with infections picked up while hospitalized outside the country, especially in the United States and South Asia, Jamal says almost a third of new CPE cases in Ontario afflict people who haven’t travelled abroad but have had exposure in a Canadian health care facility.
“It spreads within our health care system because we either don’t pick it up fast enough, or our infection prevention and control measures maybe weren’t good enough,” she says. “And then you just get local dissemination, which is the part to me that’s actually the scariest and the most interesting because the pathogen itself doesn’t really know or care where it lives.”
Jamal belongs to a network of researchers studying antimicrobial resistance (AMR) at Temerty Medicine and its affiliated teaching hospitals. They’re pushing to not only expand the state of scientific knowledge about emerging treatment-proof infections but are fighting to put the related public health issues back on the radars of policymakers.
“The World Health Organization still calls antimicrobial resistance a silent pandemic,” says Jamal. “I mean, you can spend a day in our hospitals, and there’s absolutely nothing silent about antimicrobial resistance if you come on the wards or the ICUs. We see these difficult-to-treat infections literally every single day. It’s not a future problem. It’s a problem now, so I’m not sure what’s silent about this pandemic.”
The rising tide of AMR has many and diverse causes. Certainly, the best known involves the over-prescribing of antibiotics, particularly for viral infections of the upper respiratory tract. In the 15 or so years prior to the COVID-19 pandemic, public health officials and epidemiologists sought to spotlight C. difficile outbreaks in hospitals and other congregate care settings where infectious diseases spread rapidly, either through direct contact or by airborne droplets.
But there are many other drivers of AMR, notes Scott Gray-Owen, a molecular geneticist and the director of the Emerging and Pandemic Infections Consortium (EPIC), a partnership between the University of Toronto and five major hospital research institutes.
Gray-Owen focuses his research on the bacteria responsible for rapidly progressing invasive meningococcal meningitis and gonorrhea. Until fairly recently, many public health professionals regarded gonorrhea as a disease of the past, eradicated by antibiotics, says Gray-Owen. But the growing incidence of sexually transmitted diseases in an era when HIV-AIDS is no longer a death sentence has produced new, difficult-to-treat strains, he says.
“Gonorrhea has rapidly acquired resistance to any antibiotic that’s been used against it,” Gray-Owen observes, adding that WHO estimates there were 82 million cases in 2023. “This has become a real problem to the point that it was one of three bacteria that were considered an urgent threat by the U.S. Centers for Disease Control and Prevention. This is something that has not gone away.”
COVID-19 played a curious dual role in the growth of AMR. With emergency rooms inundated with patients, many of them suffering from suspected secondary bacterial infections, Jamal says COVID-19 hugely accelerated the spread of a range of infectious diseases within health care settings, as well as the use of antimicrobials to treat them — a veritable hot house for the evolution of drug-resistant strains.
“Hospitals became overrun through the various stages of the pandemic,” says Susy Hota (MD ’02, MSc ’11, PGME ’07), an associate professor in Temerty Medicine’s Department of Medicine’s Division of Infectious Diseases, and the division head for infectious diseases at University Health Network and Sinai Health.
“That really pressured the system in terms of being able to isolate patients appropriately for the various types of infections that they had. When the hospital is so full, we no longer have isolation rooms that we would normally use to keep people who carry antimicrobial-resistant organisms separate from others,” she says. “It became less of a priority to isolate patients with antimicrobial-resistant organisms than preventing the transmission of COVID-19, which is highly contagious.”
With the intense public focus on the infectiousness of COVID-19, and the scientific fights over whether it is transmitted on surfaces, through droplets or by tiny aerosols, vast sums of funding poured into pandemic-oriented research at the expense of other priorities, among them AMR, says Jamal.
“The impact of COVID-19 on AMR has been quite devastating,” she adds, citing a 2022 CDC report noting a spike of AMR in the U.S. early in the pandemic. “To those of us who do antibiotic resistance, we knew this was going to happen,” says Jamal. “There was a massive diversion of resources from all infectious disease initiatives to COVID-19, including within our group. For a good few years we were not doing any CPE research. Nobody had the bandwidth.”
EPIC was established at U of T in 2022 to fund infectious disease/AMR research and undertake related projects, such as driving improvements to prescribing practices through stewardship programs that provide expert advice on best practices for antimicrobial use to front-line physicians.
As Natasha Christie-Holmes (PhD ’08), a longtime manager of U of T’s high containment labs, and the director of strategy and partnerships for EPIC, says, “It’s probably been 15-plus years of consistent efforts to inform the clinical community about best practices and about standards of care in terms of antibiotic use. There’s now standardized stewardship practices in a lot of major hospitals, but it’s harder in rural settings, which tend to have smaller teams and less resources.”
There’s a wide range of AMR-related research, including interdisciplinary projects that EPIC’s granting programs deliberately seek out. One area that’s attracting a lot of attention is the use of genomics and sequencing to essentially map the trajectory of an outbreak within a health care setting in real time.
“Say you had an outbreak of an infection on a specific unit in a hospital,” says Hota. “You’ve identified three patients. The microbiology lab would send their clinical specimens off to a research lab that can perform specialized molecular analysis.”
By looking at and then comparing nucleic acid from the microbes causing the infections, it might be possible to determine the relatedness of cases or a path of infection between infected patients, even if they’d never met or were in different parts of the hospital.
Hota is a co-author of a study published in December 2023 in the Journal of Clinical Microbiology that demonstrates how whole genome sequencing could be used to investigate the transmission of an antimicrobial resistant form of fungus called Candida parapsilosis in a pair of Ontario hospitals.
The authors conclude, “Timely access to genomic epidemiological information can inform targeted infection control measures.”
But, as Hota cautions, the use of this approach is still a work in progress. The task of identifying transmission patterns using genomics is highly complex because the sequencing data can be very difficult to interpret.
What AMR researchers ultimately hope to achieve, besides scientific breakthroughs, is increased recognition of the grave risks associated with the kind of pandemic that hasn’t generated enormous amounts of public and media attention, yet claims thousands of lives each year. Citing a 2019 study by the Council of Canadian Academies, Jamal notes that about 5,400 people in Canada die from drug-resistant infections each year, and the cost to the health care system now runs to about $1.4 billion annually. Countless other patients will endure lengthy and painful recoveries that may only partially resolve or leave them with permanent disabilities.
“How,” she asks, “is that not front-page news?” •
By Meagan Gillmore
Navigating the medical system with vision loss is a strange experience for me.
Unless I have my white cane out, most people — including in hospital corridors and doctors’ waiting rooms — don’t realize I have a disability.
I am legally blind, from birth. My vision is about 20/200 — the threshold for legal blindness. Simply put, if people with full vision can see objects from 200 feet away, I need to be standing 20 feet away to see the same thing.
Even then, I am likely to miss the finer details. I don’t rely on braille. I can read most print if it’s large enough and I have the right glasses with me, or if I can bring the words close to me.
Take the hospital in Brantford, Ontario that I went to for cataract surgery, in 2020 and 2023. The small font used on the signs posted around the facility confused me. The signs told me which hallway led to the unit where my surgery would take place. They told me what information I needed to give when I checked in for the surgery. And, I struggled to read them.
I viewed the building around me with a skeptical, perhaps cynical, journalistic eye.
I wondered about the hospital staff. I’m here for eye surgery, I thought. Shouldn’t they automatically have large print?
Then I remembered: I was not at a medical facility devoted to eye care. Most people who come here could read the sign in front of me and all the other ones that blurred by me as I travelled the hallway.
There’s a public perception that those of us who have significant vision loss rely solely on our sense of touch. That isn’t necessarily true. Likewise, it’s not true that my vision loss is the main medical fact about me. Yes, most of my doctor’s appointments are for my eyes. But my eyesight has remained stable for most of my life. When my ophthalmologist touches my eyes, it’s during surgery when I’m heavily sedated and unable to know what’s happening. But at a medical appointment not related to my eyes, I may forget to mention my visual impairment and the assistance I may need — assistance that could, presumably, include touch.
Navigating by touch can be complicated when visiting doctors or health-care facilities, like hospitals. But perhaps establishing connection doesn’t have to be.
People like me, who have had impaired vision since infancy, are fairly rare. Vision loss — like disability generally —increases as people age.
People with vision disabilities account for seven per cent of Canada’s population. It’s predicted that vision loss will increase dramatically in the next decade. In the decades ahead, data indicates that more people with a vision impairment will be using the medical system.
According to Statistic Canada’s 2022 Canadian Survey on Disability, disabilities that relate to sight are the fifth most-common reported disability type; 27 per cent of the people who reported a disability that limits their daily activities reported one related to vision.
To address this surge, Parliament is considering creating a national vision health strategy. A bill requiring the minister of health to develop a national strategy to support the prevention and treatment of eye disease, and vision rehabilitation, has been in the Senate since October 2023. The vision health strategy, as proposed, focuses specifically on eye disease and vision loss.
It includes identifying, in the words of the bill, “the needs of health care professionals and other professionals in relation to training and guidance on the prevention and treatment of eye disease and on vision rehabilitation.”
Helping doctors treat patients with disabilities isn’t easy. For one thing, disabled patients may not talk about how their disability impacts their experience with the medical system. Admittedly, when I’m going to see a doctor who isn’t an eye doctor, I rarely think about my visual impairment once I’ve figured out a way to fill out the forms. For another, doctors may never have had a patient who is visually impaired or blind.
If a patient has a disability, it’s important “to acknowledge it rather than pretend it doesn’t exist,” says Radha Kohly (PGME ’09), the vice-chair of clinical services and wellness at the Temerty Faculty of Medicine’s Department of Ophthalmology and Vision Sciences, and a medical retina specialist at Sunnybrook Health Sciences Centre.
“Don’t make an elephant in the room when there doesn’t need to be one,” she says.
Most of Kohly’s patients are seniors, but their ages have ranged from 18 to 102. Very few patients mention how their vision loss impacts their other medical experiences, she says. Acknowledging the patient’s disability may be the first step in doctors connecting with patients, she says, and ultimately improving health care for patients with vision loss.
“Touch can be an essential part of medical care,” says Kohly. She recommends that doctors tell patients with vision loss what they’re going to do before they do it.
Providing good medical care — care that connects — with patients who have disabilities begins with rethinking disability, says Audrey Yap (MScCH ’10), the accessibility theme lead for Temerty Medicine’s MD Program and an assistant professor in Temerty Medicine’s Department of Medicine. Yap and Janet Rodriguez, a patient mentor and disability justice advocate, work together on the curriculum, which is based on disability inclusion and anti-ableism principles.
Doctors need to shift their perspective and stop thinking about disability as a problem that needs to be fixed, says Yap. For her, this means viewing disability as a normal part of the human experience. It has also meant changing her thinking.
“It’s not that patients with disabilities need a longer time,” says Yap, who is also a physiatrist at Hennick Bridgepoint Hospital, which is part of Sinai Health. “It’s that they need enough time.”
Rushing through an appointment instead of providing the right treatment to a patient would not be providing good patient care, she says. Some patients’ disability makes touch painful. In these cases, communication between patients and doctors is especially important.
Rodriguez, who has had rheumatoid arthritis for 30 years, volunteers as a patient partner to help teach Temerty Medicine residents and learners how to do a musculoskeletal screening exam alongside a rheumatologist. In the exam, doctors need to touch Rodriguez’s joints to see where her pain is, but touch will hurt. Putting pillows underneath a patient’s arms or elbows can help alleviate some of the pain, says Rodriguez. So can pressing down on a joint very lightly. Doctors “don’t need to linger,” she says. But they need to listen to her.
“I will never compare my knowledge to that of my rheumatologist or my surgeons; they are the experts,” she says. “But when it comes to the illness and the journey of my health and wellness with the illness, or the illnesses, that is me.”
Rodriguez makes an important point. For me, it can be natural to assume that I am the only person involved with my disability, but I’m not. The medical system and the people who comprise it are also part of it. Their skills matter. I hope to live a long and healthy life, and I know this likely means that I’ll see doctors for many reasons not related to my eyes. Even when touch is absent, I hope there can be connection, based on humility and mutual respect. •
By Blake Eligh
Working without scans or X-rays, physical therapists rely on their hands to tell them what lies beneath the skin. With their fingertips, they trace the line of a tendon, probe the edge of a kneecap, or cup an elbow joint to feel for the telltale swelling or warmth that indicates an injury.
Touch is an invaluable tool in Tricia Twogood’s work as a physical therapist and assistant professor in the Temerty Faculty of Medicine’s Department of Physical Therapy.
Tricia Twogood (MScPT ’09) primarily treats musculoskeletal conditions in her clinical practice, providing physical therapy for patients who may have multiple diagnoses, such as a history of cardiovascular disease or stroke, and previous injuries. She depends on touch to confirm a diagnosis and during therapy as she works to bring her clients’ attention to a specific body part or movement.
“Touch is fundamental to what we do and who we are as physical therapists,” she says.
But our broad understanding of the sense of touch is only just beginning to be understood. In 2021, California-based researchers Ardem Patapoutian and David Julius won the Nobel Prize in Physiology or Medicine for their groundbreaking research in sensory biology.
Patapoutian, a molecular biologist at San Diego’s Scripps Research, identified Piezo1 and Piezo2, the pressure-sensitive channels crucial for detecting the pressure of touch. Julius, a physiology professor at University of California San Francisco, discovered a nerve cell protein that responds to high temperatures.
Their independent yet complementary studies shed light on the fundamental physiological process underlying the perception of touch, pressure, temperature and pain.
It’s something that drives the work of neuroscientist Min Zhuo, a professor in Temerty Medicine’s Department of Physiology. Zhuo, who holds the Michael Smith Chair in Neuroscience and Mental Health, studies the relationship between pain and cognition.
Zhuo’s research shows that emotions such as fear and anxiety can activate chronic pain by releasing a surge of neurotransmitters from the brain’s frontal lobes to the spine. His research highlights the crucial role of the anterior cingulate cortex (ACC) in processing and regulating sensory and emotional experiences related to acute and chronic pain.
Thanks to ACC, how the brain registers touch and pain are closely intertwined, he says. When someone touches your hand, the mechanical stimulus triggers tiny electrical signals that travel through the body’s somatosensory system. The signals move from skin to spinal cord, where glutamate neurotransmitters relay the information to the brain’s cortex for conscious perception. This process, known as ascending sensory transmission, loops in the visual centre to recognize the touch and its source, and activates ACC in the process.
“Human imaging studies show that the ACC is activated if you have an injury or suffer an acute pain, like burning a finger,” Zhuo says.
By activating the body’s emotional response, the neurons become conditioned to respond and can increase or suppress the brain’s response to mechanical stimuli, including touch.
“For people with chronic pain, like neuropathic pain or spinal cord injuries, this ACC activity may enhance or even cause a pain response,” he says. “When circuitry is highly activated, even a gentle touch can trigger a strong response.”
This emotional response of ACC can also influence how the brain responds to touch, Zhuo says.
“If it’s the touch of a friend, or a lover touches your hand, the brain will understand this and respond accordingly. If the touch conveys dangerous information, the brain will amplify the sensation and cause you to withdraw your hand,” he says.
“The body’s system produces feedback control in response to peripheral sensory stimulation. It can make the whole body become super-sensitive to touch.”
As researchers unravel the science of touch at the molecular level, questions remain about the role of touch in social situations, including clinical settings.
This is an area of practice that Pier Bryden (PGME ’97, PGME ’01) has often considered in her work as a staff psychiatrist at The Hospital for Sick Children and as Temerty Medicine’s associate dean of clinical affairs and professional values. Bryden says that touch can be a delicate subject in health care, especially when it comes to interactions with young patients. Training has traditionally discouraged nonclinical touch between practitioner and patient, even when a child actively seeks comfort.
“In my practice as a child psychiatrist, I would never initiate nonclinical touch of any kind,” she says. “A child may not be able to tell me if they don’t like it, or they may be intimidated by the fact that I am an adult and a doctor. A significant number of child and adolescent psychiatry patients may have histories of trauma, so when it comes to touch, we are very careful.”
However, Bryden notes, there are times when touch may be appropriate or even necessary. She points to the work of Austrian psychoanalyst René Spitz, whose post-war study of children raised in foundling hospitals revealed the critical role of touch in a child’s physical and emotional development.
“The children who weren’t touched were significantly developmentally delayed, which raised the question of what children need [in order] to develop — social interaction and, arguably, touch,” she says. The answer to the question of contact with patients requires reflection, says Bryden.
“What do you do when a young child gives you an unexpected hug or asks for comfort?” she asks. “Particularly with younger children, you have to consider what rejecting touch means and how cognitively capable they are to understand the rationale.”
Bryden recommends preparing boundary-setting phrases that offer a neutral option.
“I might say, ‘I’m more of a handshaker’ or offer a high-five,” she says. “But there are times when I’ve been taken off guard, and rejection would be significant. Sometimes you have to make in-the-moment decisions.”
In residency training, Bryden notes that there are clear lines around consent and communication.
“You cannot touch someone without first explaining the purpose,” she says.
Bryden points out that complaints to medical oversight boards often cite practitioner touch that the patient didn’t feel adequately prepared for. The College of Physicians and Surgeons of Ontario’s “Boundary Violations” and “Advice to the Profession” documents set out clear physician obligations in such interactions.
“Patients might not know they would be touched in that way, when it was coming or were taken by surprise because the physician didn’t take the time to explain it,” Bryden says, adding that the more intimate the exam, the more important it is to explain what you will be doing and why, and to get patient consent.
Bryden says it’s critical to discuss scenarios in training and prepare boundary-setting phrases to offer a neutral option. For example, if a paediatric patient asks for a hug, Bryden suggests that practitioners can take cues from their relationship with the family. If a hug is provided, it is with explicit consent and in the safety of a public space.
“The younger they are, the more you have to be guided by parents. It should always be in public — never in private — for me, that’s an absolute. Preferentially, it should be observed by parents, and the longer you have known the patient and the family, the better,” she says.
The issues that Bryden brings up are also on Twogood’s mind. For Twogood’s learners, who will rely on touch as part of their practice, navigating these areas is a skill that must be learned.
“It can be a very big deal to make physical contact with another person, and physiotherapists must never lose sight of this,” she adds. “It’s a huge part of the training for the students I work with.”
Equally important are consent and communication.
“In practice, the early part of our encounters always begins with a verbal conversation, and then there is the transition to physical contact,” says Twogood. “There isn’t a recipe for how that occurs — it should be a dialogue between the patient and the practitioner.”
For Twogood, it’s undeniable that touch plays an integral part in clinical practice. Clients may hold themselves differently when touched, standing up a little straighter or moving differently, she adds. “Touch changes the dynamics of the social interaction.”
There are also times when Twogood strategically withholds or removes touch to deliberately reduce the amount of feedback she is providing while a client practises a movement or exercise.
“Clients may not remember a lot of what we tell them,” she says. “If I really want someone’s attention, I might pick the moment that I am touching them to deliver certain information.”
Ultimately for Twogood, the role of touch is greater than the sum of physiological or anatomical parts.
“Touch changes the dynamics of the social interaction,” she says. “It goes beyond mechanics and anatomy. As physiotherapists, we are deliberate about targeting specific tissues of the body when we use touch in clinical practice, but at the end of the day, it’s also a connection between two people.” •
Touch is a form of human connection. When I think of touch, I think of one person touching another to give them protection and connection, and to share an experience. In neonatology, when we celebrate the birth of a child, we hug the parents. Even though we are physicians, we still celebrate their celebrations, or at least I do. Sometimes, I ask, “Is it OK if I hug you?” And I’ve never been told no.
On the other hand, touch can be incredibly important during the death and dying process. In neonatology and critical care, we deal with death and dying at a time that’s supposed to be a time of celebration.
The loss is not just the loss of a baby who is very sick, it’s the loss of everything the family envisioned for what the baby would experience. A little girl, a little boy, soccer, ballet. That loss is tremendous and being able to touch someone shows them, “I get it.” Touching and hugging someone, and being there with them, can connect us in a way that words can’t.
When I am working with trainees, one of the questions I ask is, “Did you examine the baby?” Sitting and looking at the computer at all the vital signs, or the quotes from the nurses, never replaces actually going to the bedside and examining the baby.
In medicine, to provide care to patients at the most vulnerable times in their lives requires active listening to their story, as well as examining and touching the patient. These actions personalize the patient-doctor relationship and say, “I believe you, and your journey to recovery is our journey together, hand in hand.”
_
Estelle Gauda is a professor in the Temerty Faculty of Medicine’s Department of Paediatrics, and the Department of Laboratory Medicine and Pathobiology. She is also head of The Hospital for Sick Children’s neonatology division and the Women’s Auxiliary Chair in Neonatology at SickKids.

PIEZO1 and PIEZO2 are proteins that control signalling in our body. As ion channels, they help plants, animals and humans to feel touch, in cells, tissues and organs. The reason we feel touch — or even pain — is because of mechanical force. PIEZO1 and PIEZO2 are required for cells to sense force.
The reason I am interested in this area is that I want to help brain cancer patients. That’s my passion. I also want to study a less explored area. At my lab, we study how these proteins control tumour growth.
People say there is a marriage between biology and chemistry. But I see much less development in the research that combines biology and physics. Some of the first things we learn about in physics are force and how objects react to force. Yet, there is a very limited understanding of what type of forces exist and how much force there is in brain tumours. We also need to learn more about how tumour cells and non-tumorous cells (like immune cells and neurons) sense and respond to force.
To me, it’s a black box. I want to connect the dots between mechanical force, force sensors and cancer, and develop new ways to treat brain cancer and help patients.
_
Xi Huang is an associate professor in Temerty Medicine’s Department of Molecular Genetics, and a senior scientist in the developmental and stem cell biology program at The Hospital for Sick Children. He holds the Canada Research Chair in Cancer Biophysics.

I am a physiotherapist who works with patients who have had a stroke. They can range in age from 18 or 19 years old, to those who are more than 100 years old. All of the patients we work with have had something life-changing happen. Stroke can be a very devastating event.
Part of my work has focused on normalizing conversations about sex for people who have experienced a stroke. In the past, it was really noticeable that there was a large gap in our practice, where people felt like talking about sex after a stroke but thought it was a taboo topic. Patients and caregivers didn’t feel comfortable opening up with us about sex. In terms of touch and intimacy and sex, there is a whole connection piece that is a big component of recovering from a stroke.
We wanted to normalize the topic and make sure people had the opportunity to address the subject if they wanted to. In stroke recovery, we’re good at asking about goals. We work in rehabilitation, so we ask, “What are the things you need to do to go home?” So, from a goals perspective, you’ll hear answers like, “I need to go to the bathroom myself.” Or, “I need to feed myself.” Or, “I have to walk.”
To help people feel more comfortable talking about stroke recovery and sex, we created education pamphlets for patients and posters for the walls. We also incorporated talking about sex into our goal-setting interview for all patients. These changes have made a big difference in the care that we provide, and we’re getting more comfortable with the topic.
After a stroke, your life can look very different. As health care practitioners, we have to be very mindful not just of the health impacts of a stroke, but also how the stroke affects the patient in the roles and relationships they have with the other people in their lives. And, we can influence how patients preserve and foster those relationships by opening up these discussions.
_
Vanessa Ong is a clinical instructional assistant in Temerty Medicine’s Department of Physical Therapy and a physiotherapist at University Health Network’s University Centre.
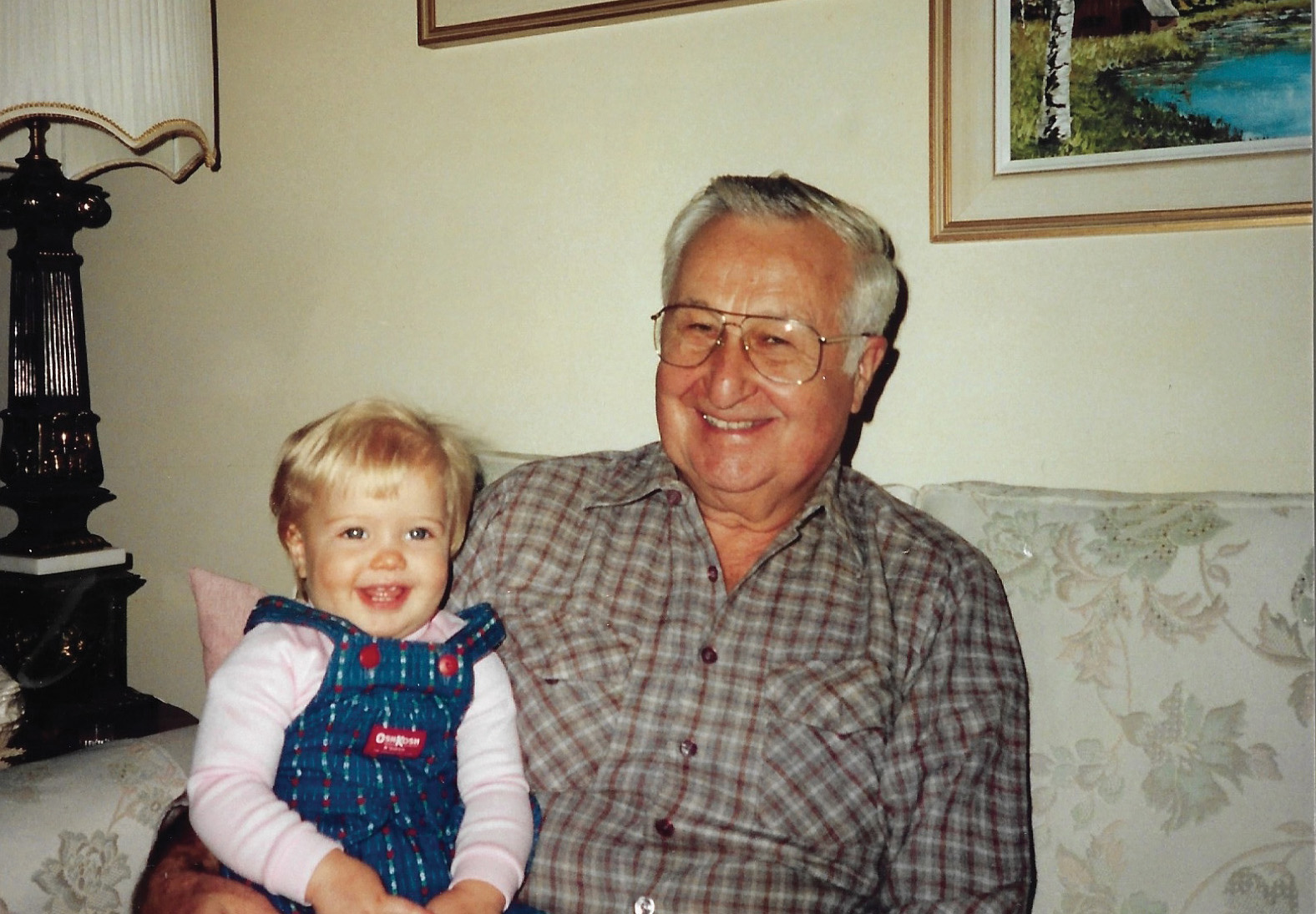
Laura Hensley, and her grandfather, John Hlavach
By Laura Hensley
My grandfather died the way he wanted: at home in Toronto, in his bed, holding my grandmother’s hand. They’d been married for 72 years.
My grandfather had been suffering for months, his body steadily declining as prostate and lung cancer consumed him, cell by cell. In his final months in 2020, he didn’t do much moving. He couldn’t walk, and at the height of the COVID-19 pandemic there weren’t many places to go, anyway.
I’d kept my distance from my 94-year-old grandfather in the weeks leading up to his death, terrified of passing on a virus that disproportionately killed older people. But when his palliative doctor told us he had only days left to live, I wanted nothing more than to hold him, touch his hands, his head and his arms. Due to high doses of pain medication, he was unable to communicate as he normally would, so I wanted to make sure he knew I was there. If he was going to die, I thought, why not make sure he felt his family around him? I am not a trained scientist but on an intuitive level, I know touch is important.
Touch is one of the first senses we develop in the womb. Throughout our lives, feelings on our skin activate our nervous system and send signals to the brain. The right kind of touch has healing capabilities. Massage, for instance, has been shown to help with the symptoms of conditions such as arthritis, multiple sclerosis and Parkinson’s. It might also help lower blood pressure. Touch therapies, such as massage and reflexology, have been shown to improve both the physical and emotional symptoms of cancer patients, including lessening their pain and fatigue.
Touch is an unparalleled way to communicate with people — especially those like my grandfather who, before he died, was no longer able to speak — and to tell them, “It’s OK, you are safe, I am here.”

Breffni Hannon (PGME ’13, MSc ’18), an associate professor in the Temerty Faculty of Medicine’s Department of Medicine and a palliative care site lead at Princess Margaret Cancer Centre, says that during her career, she has seen how powerful touch is for people who are close to the end of their life.
“I have seen patients be so comforted by having their families able to sit close to them, lay beside them, hold their hands and embrace them, including patients who were restless or agitated,” Hannon says. “It’s the art of human connection.”
There’s an emphasis on touch at the beginning of life, she says, when parents are encouraged to engage in skin-to-skin contact with their newborn. For example, touch can facilitate bonding and secure attachment between a baby and their parents, as well as create a sense of safety in a child — which is key to psychosocial development. Then, as kids grow, research suggests that affectionate touch (which promotes the feel-good hormone oxytocin) can lower stress levels and promote healthy social engagement.
In other words, touch grounds us. As we age, however, we may move away from the frequent touch we had in childhood. For older adults, hugs with friends might be less common. For those without an intimate partner or close family, the act of cuddling or holding hands may be rare. During the COVID-19 pandemic, for example, the term “touch-hunger” was introduced — a new way of acknowledging that physical touch matters.
Then there is the experience of death. When someone is dying, Hannon says touch can become more of a “medicalized” experience — like when a patient has an IV tube inserted into their arm, or they’re hooked up to a ventilator. This makes a more personal kind of touch even more important — which can be used in tandem with treatment, says Hannon.
“Touch really helps patients to be more relaxed,” Hannon says. “You see it in their facial expressions, in their breathing and how they hold their bodies. All of these physiological markers show just how important touch can be in the end-of-life experience.”
Seana Bulle, a second-year family medicine resident at Temerty Medicine, says that it’s paramount to deliver the best end-of-life care, making patients feel comfortable and abiding by their wishes. She says a lot of patients will say that their family is important to them and that they want to be surrounded by their loved ones as they die. The role of touch in this situation offers a sense of familiarity.
“Touch can be a love language used in various cultures. It can bring a grounding presence to patients who are at the end of their lives, or who have serious illnesses,” Bulle says. “Touch can be calming and allow the patient to feel surrounded by loved ones.”
Bulle has worked in a variety of environments with patients who are at the end of their life, including in hospitals, homes and hospices. She has found that the connecting thread in her work is that good experiences need to focus first on the patient’s needs. That means that health care providers must really understand who a patient is and what matters most to them.
“In palliative care, we ask questions that I don’t see routinely asked in other medical specialties, such as, ‘What are you worried about in the future?’ Or, ‘What are you hoping for?’ And my favourite, ‘What do we need to know about you as a person in order to provide you with the best care possible?’” says Bulle, who is beginning a year-long fellowship in palliative care at the University of Toronto next month.
Culturally relevant palliative care is also crucial, says Bulle. When health care providers understand a patient’s background, family history, religious beliefs and end-of-life desires, they can aim to deliver the best experience for them, she adds.
Bulle also says that not all Canadians have equal access to palliative care; research suggests that people of colour and recent immigrants may have poorer access. In Canada, palliative care has historically been rooted in Eurocentric ideologies, Bulle says, and, as a result, hasn’t always included racialized groups and their specific needs.
“It’s really important for us to understand how we can help support these various groups and how their needs may change depending on what their experience and background is,” she says.
Quality, patient-centred end-of-life care isn’t just a benefit to patients, Hannon says. Being physically close to a person as they’re dying, whether that be in the home or in a medical setting, can be a comfort to the family, too. Hannon says there’s often a feeling of hopelessness for family members when a loved one is about to die, and a feeling of helplessness if they can’t contribute to their medical care. Touch is a tangible way to help the person who is dying — and their loved ones — feel soothed.
“To me, the physical presence of a loved one is far more valuable in many instances than a doctor at the end of somebody’s life,” Hannon says. “I think it also allows the loved one to feel like they’re part of the care team.”
This was certainly the case for my grandmother during my grandfather’s final months, and for me during my grandfather’s final days.
In September 2020, I camped out at my grandparents’ house for the three days before he passed away on September 28. I kept a mask on when I was near him, still afraid of passing on a virus, even though his body was starting to shut down. The focus had shifted to managing his pain and making him as comfortable as possible.
It brings me solace to know that when my grandfather passed, he was in his bedroom, in the home he had lived in for the last 65 years, as my grandmother grasped his hand and sang him a song. I cried because I had just lost him. But I also smiled because I knew he felt at peace. I gently kissed his forehead knowing it would be the last time I would be able to physically touch him.
A few days later, my grandfather was cremated on my birthday, exactly 30 years after he first met me and cradled me in his arms. My mother told me that as soon as I was born in the hospital, he couldn’t stop holding me. I think back now and am grateful knowing that his soft skin was some of the first that my newborn body felt.
And, I sleep easy knowing he left the world the way I entered it: feeling the warm touch of someone who loved him very much. •
Laura Hensley is a Toronto-based writer and journalism instructor.

By Hilary Caton
As a mother of three kids under the age of seven, Dani Seligman is no stranger to stitches, fractures and scrapes. But she doesn’t let her kids’ past fumbles make her fearful of their outdoor activities at the local playground. Seligman is a big fan of unstructured free play — an approach she acknowledges isn’t always shared by some of her more cautious peers.
“I know it sometimes feels unnatural for parents not to be fearful of their child hurting themselves,” says Seligman. “But part of parenting is also about us learning how to judge our own feelings and reactions, so that we know when to intervene or not to intervene.”
Seligman isn’t alone in her belief in risky outdoor play and unstructured free play. Experts are also paying attention.
Take a 2023 finding in the Journal of Pediatrics, which concludes that one of the main reasons for the rise in youth mental health issues is the drop in “opportunities for children and teens to play, roam, and engage in other activities independent of direct oversight and control by adults.”
Then came a 2024 position statement from the Canadian Paediatric Society (CPS) encouraging caregivers to ditch overly supervised play for more opportunities for children to engage in outdoor free play, particularly risky free play.
So, what’s with the explicit advice that hands-off parenting is needed?
“There is increasing research that has come into the forefront recently on the loss of outdoor, free and risky types of play that used to be so common and prevalent. This loss is felt to be impacting the rising rates of mental health conditions that we are seeing in children, and the rising rates of obesity, anxiety and behavioural disorders that are potentially connected to a loss of risky play,” says Suzanne Beno, an associate professor in the Temerty Faculty of Medicine’s Department of Paediatrics and co-author of the CPS position statement. Risky play is described in the statement as “thrilling and exciting forms of free play that involve uncertainty of outcome and a possibility of physical injury.” (Risky play is not to be confused with hazardous play, in which “the potential for injury is beyond the child’s capacity to recognize it as such or to manage it.”)
“We’ve become so supervised, and so structured, and so precautionary. There’s been such a shift away from unstructured free play, and there’s so much value to that type of play,” says Beno. “What prompted us to write this position statement is that there is an increasing amount of research demonstrating the significant value and loss that our kids are experiencing from not being exposed to risky play anymore. We really needed to make the statement that kids need to be as safe as necessary, rather than as safe as possible.”
An increase in “helicopter parenting” — a term first coined in 1990 to illustrate how parents may hover, metaphorically, over their children, ready to swoop in and rescue them from disappointments, painful experiences and the dangers of the world. But this hovering can have a negative impact on a child’s mental health.
According to Ripudaman Minhas, an associate professor with Temerty Medicine’s Department of Paediatrics, children lack independence and have fewer opportunities to spread their wings, and experiment and learn from their mistakes.
“There may be less risk-taking, and less opportunities to try and learn new things. There may also be difficulty in coping when situations aren’t successful,” says Minhas, who is also the principal investigator of the Our Kids’ Health Network and a developmental paediatrician at Unity Health’s St. Michael’s Hospital.
What parents may not realize is that there are multiple benefits for children when caregivers learn to let go and allow unstructured play to happen, according to CPS. By encouraging risky free play, parents may be increasing their child’s physical literacy, and the mental health benefits may include greater resilience, better conflict resolution and problem-solving skills, and higher self-esteem.
Their social-emotional health may also increase, which includes a child’s ability to communicate, cooperate and compromise. It gives them opportunities to experiment with uncertainty and develop coping strategies, which can significantly reduce a child’s risk of elevated anxiety, according to the CPS statement.
“Children need to learn how to regulate themselves through times where there may be feelings of failure. They need to have the tools to cope with things that may not go as initially planned. Those are important things to learn early on so that they have these skills as adults, and helicopter parenting can hinder that development,” says Minhas.
Emerging evidence suggests that “overprotective and controlling” parenting may possibly lead to increased anxiety, depression, prescribed medication and recreational consumption of pain pills, according to a report in Frontiers in Psychology. It has also been linked to a decrease in well-being, self-regulation, self-efficacy and poorer academic achievement, according to an article in the Journal of Child and Family Studies.
Brendan Andrade, an associate professor in Temerty Medicine’s Department of Psychiatry and a senior scientist with the Centre for Addiction and Mental Health, says it’s important not to rest the blame squarely on the shoulders of parents for discouraging free play.
“There’s no fault here,” Andrade says. “They’re doing what they think is best for their child to keep them out of trouble, or to help stop them from hurting themselves,” Every situation is unique, he adds, but ultimately it’s about, “parents trying to do what they can to meet their children’s needs.
“Sometimes when kids have higher degrees of needs or sometimes when there’s environments or situations that are problematic, parents do what they think makes sense,” continues Andrade. “They’re typically doing it with the best of intentions. But sometimes even the best intentions may result in something that’s unintended.”
Simple things such as allowing children to fill boredom with their own interests can be important, says Minhas, adding that it’s crucial for a child’s development to have unstructured time.
“It’s important to position the parenting journey as being something where you’re slowly passing the baton on to the child in terms of incremental tasks where they get to take more of a lead,” adds Minhas. It also means giving children the opportunity to explore and to develop abilities in a play situation that sometimes doesn’t involve parents at all, he says.
“One of the things that’s important for parents to think about is giving the child the opportunity to get through their experience of emotional distress in a way that’s supported or coached,” explains Andrade. “It’s important for kids to be able to test their own limits, to be able to develop their own problem-solving skills and their own capacity to tolerate distress and work through it. Risky play allows them to do just that.”
That advice rings true for Seligman.
“When we make all of the decisions for the kids, it really doesn’t allow them to develop that skill set which they will need for later in life for the things that will have bigger repercussions,” she says. •

By Emma Jones
The late Ian Copland (MSc ’00, PhD ’06) was known as an uplifting force to the many people whose lives he touched.
“We called him ‘Mr. Neighbourhood’ because he would engage in conversation with anybody,” says Ian’s widow, Jenn Copland. “He was a goofball and super funny and so warm. I am still meeting people who were influenced by him.”
Ian unexpectedly died on July 15, 2015, following a sudden cardiac arrest while playing hockey — a sport he had loved since childhood. He was only 42 years old.
In life, Ian had a vivid presence and a brilliant mind. A dedicated family man, Ian and Jennifer shared two children, Matthew and Samantha, and were close with Ian’s parents, Bill and Susan Copland, and Ian’s siblings Heather, Meagan and Andrew.
Ian had completed both a master’s degree in physiology and a doctorate in molecular biology at the University of Toronto’s Faculty of Medicine — now the Temerty Faculty of Medicine.
Martin Post, a professor of paediatrics and physiology at Temerty Medicine and a senior scientist at the SickKids Research Institute, supervised Ian’s PhD research, which explored the ventilator’s role in causing lung damage in premature infants. Post remembers how Ian always centred his scientific work on the impact it could ultimately have on patients.
“He always had an eye out for how research could be applied and lead to new therapies,” says Post.
After finishing a postdoctoral degree in Montreal in 2008 with Jacques Galipeau — now the assistant dean for therapeutics discovery and development at the University of Wisconsin School of Medicine and Public Health — Ian was offered a role as an assistant professor of hematology and medical oncology at Georgia’s Emory University. There, he pursued research on the mechanisms that regulate how particular cells promote tissue regeneration. True to his passion for translational science, Ian also co-founded Cambium Medical Technologies shortly after starting at Emory. The company, which continues to operate today, uses blood-derived products in regenerative medicine.
Before his death, Ian’s scientific career was flourishing. He was athletic and showed no signs of discomfort in the days and weeks prior to his passing. The news of his death came as a shock to his family, friends and colleagues.
While Ian’s cause of death is unknown, it is believed he had a cardiac arrhythmia, in which a person’s heart beats outside of its usual rhythm because of faulty electrical signalling. Children and adults with an arrythmia often do not experience any warning signs.
Michael Gollob, a professor of cardiology and physiology at Temerty Medicine and the research director of Toronto General Hospital’s Inherited Arrhythmia and Cardiomyopathy Program, explains how the cause of sudden, dangerous arrhythmias has been a mystery until recently.
“New advances have shown that many of these conditions are caused by genetic abnormalities which impact the heart’s electrical function — which can lead to sudden, erratic electrical activity of the heart causing a cardiac arrest,” says Gollob.
Ian’s death left his family heartbroken but also determined to continue the arc of scientific discovery to which he was so dedicated. In 2023, members of Ian’s family made a generous gift to establish the Ian Copland Accelerator Fund in Inherited Cardiac Arrhythmia Research at Temerty Medicine.
The gift will honour Ian’s memory by paying tribute to his passion for the transformative impact of fundamental health science by supporting pioneering investigations into the genetic causes of heart arrythmias.
“Losing Ian was incredibly hard for everybody,” says his mother, Susan. “We want to help prevent this from happening to another family.”
The Ian Copland Accelerator Fund in Inherited Cardiac Arrhythmia Research will help support Gollob and his team as they explore new areas related to inherited arrythmia conditions.
The Gollob Lab has made it their mission to better understand the underlying genetic causes of inherited arrythmia conditions. This is done using exome and genome DNA sequencing to compare genetic data of healthy people with patients at risk of inherited arrythmia conditions in the hopes of identifying genes and proteins that could provide the foundation for effective drug and gene therapy.
“The Ian Copland Fund provides invaluable support for critical research staff and infrastructure — speeding and strengthening our work,” says Gollob.
Susan says she sees Ian in the members of the Gollob lab, whose passion for translating their research into preventive treatments is obvious to anyone they meet.
“The work the researchers at the Gollob Lab are doing and the love they have for it is so inspiring,” says Susan. “It makes us feel that we’re really going to be able to make a difference.” •

By Heather McCall
Surgeon Rajiv Singal has seen the future, and for his patients — it’s robotic.
In his almost three-decade career, Singal (MD ’90, PGME Urology ’95) has witnessed firsthand the evolution of minimally invasive technology in surgery, beginning with laparoscopy — using small incisions and a camera to aid in treating target areas — through to the latest innovations in surgery that involve complex robotics.
In popular culture, robots are pictured on a factory assembly line or running amok in a science-fiction movie. But for Singal, robots have a practical application. In robotic surgery, the surgeons sit at consoles away from the operating table and remotely control robotic arms, he explains, adding that during procedures, they remain very much in control of the surgery.
“A casual observer may think the robot is just that — a machine that’s working away, and I’m sitting in the corner and watching it. But that isn’t correct,” says Singal, a urologist, the chief of surgery at Michael Garron Hospital and an associate professor in Temerty Faculty of Medicine’s Department of Surgery.
“The robot is the evolutionary extension of a laparoscope,” he says.
Singal, who is also the director of the hospital’s robotic surgery program, uses the robot for prostate cancer surgery and plans to start using it for kidney cancer surgery later this year. He says that using robots for surgery holds immense promise — and can lead to better patient outcomes. For example, at Michael Garron, patients are not prescribed opioids after receiving robotic prostate surgery because the pain can be managed by weaker medications that pose less risk of abuse.
However, there are limitations to robotic surgery. Singal notes that the robot can’t quite replicate the sensations that surgeons experience during open surgery, of feeling tissue between their fingers. To compensate, Singal is translating years of tactile feedback to what he sees through the console.
“When you get more experience on these robotic platforms, you learn to feel with your eyes,” he says.
This lack of haptic feedback — and the challenge it presents to new surgeons during training and in their early careers — is behind Singal’s drive to create a training tool that will synthesize virtual reality and minimally invasive surgical procedures.
At a school fair in 2016, Singal was introduced to an early iteration of the technology by Ben Sainsbury, then a PhD computer science student at Ontario Tech University. The two founded Marion Surgical and immediately started developing their first product.
The Marion Surgical Simulator, introduced in 2019, allows surgeons to plan and practise laparoscopic and endoscopic procedures, such as removing kidney stones, without any risk to patients. Users don an Oculus VR headset and use a specially designed program and custom wand to virtually recreate the operating room environment and surgical situation.
Singal says that the tool can provide haptic feedback to simulate in-surgery sensations, such as the resistance of skin that a surgical trainee is puncturing to reach a kidney stone. His team at Marion Surgical is now working to apply this haptic technology to a robotic surgery simulator that will extend beyond laparoscopic procedures.
Singal expects the future of medicine will mean the use of more robotic surgery in medical settings and virtual-reality training tools in medical schools. However, he says they will never replace the need for surgeons to have more than technical skills.
“What I value most, and what we recruit, are surgeons who embrace all of the elements of what it takes to be a good doctor,” says Singal. “We need to serve the needs of patients in our community, and that starts and ends with basic care.”

This photo, taken in about 1917, is from the University of Toronto Archives, which indicates it’s of physiotherapists in Hart House working with wounded veterans from the First World War.
In Partnership for Excellence: Medicine at the University of Toronto and Academic Hospitals, author Edward Shorter writes, “In 1917, the Military Hospitals Commission established a six-month program using Hart House as its temporary base, called the Military School of Orthopaedic Surgery and Physiotherapy, to train physiotherapists. Thousands of injured veterans were returning to Canada in need of rehabilitation treatment that as yet had not been created.”
The school, led by Lt. Col. Robert Wilson, offered three subjects: muscle function training, gymnastics, and massage and electrotherapy. According to sources that Shorter cites, 250 people finished the six-month course before practising in military hospitals across the country. The course continued until 1919. •